Case Illustration: Michael, 67 Years Old but Functionally Younger
Michael, a 67-year-old patient with venous insufficiency, demonstrated physical function comparable to a much younger individual. Objective measures showed:
Gait speed: 1.1 m/s (normal or above average for his age)
Grip strength: 34 kg (above frailty thresholds)
Lower-body power: 2.7 W/kg on a 5-rep sit-to-stand test (PowerFrail app)
Post-procedure, Michael quickly resumed active tasks, illustrating that chronological age alone underestimated his functional capacity and recovery potential.
Limitations of Chronological Age
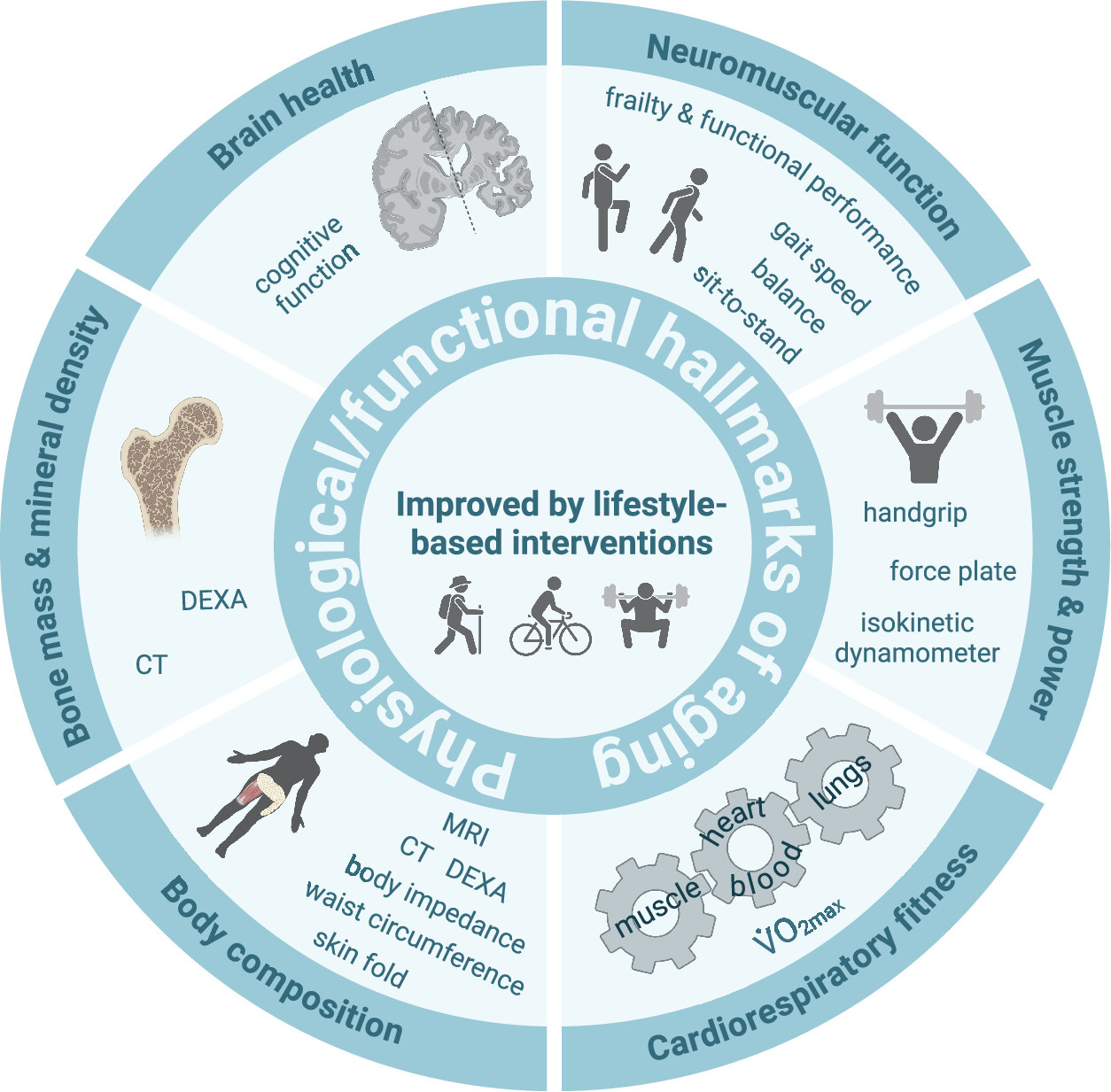
Chronological age remains embedded in insurance policies and electronic medical records but poorly predicts individual health outcomes. Research shows discrepancies of 20+ years between chronological and biological age, with functional measures correlating more closely with mortality and morbidity.
For example, a pooled analysis of 34,485 older adults found that every 0.1 m/s decrease in gait speed increased all-cause mortality risk by 12% (Studenski et al., 2011). Similar predictive value exists for grip strength, muscle power, telomere length, and epigenetic clocks.
Clinical errors from relying on chronological age include:
Undertreating robust older adults
Overtreating biologically older younger patients
Functional Deficits Drive Clinical Outcomes
Functional impairments, not age per se, predict clinical trajectories. For instance, low preoperative grip strength is linked to a fourfold increase in postoperative pulmonary complications (Yoshida et al., 2020). Slow gait and low sit-to-stand power predict longer hospital stays and higher readmission rates (Kim et al., 2020; Kunadian et al., 2019).
Despite requiring less than 2 minutes to perform, these tests remain underutilized in clinical practice.
The Two-Minute Trio: A Practical Biomarker Toolkit
Why include muscle power?
Muscle power declines earlier and faster than maximal force. A 10-year cohort study showed knee-extensor power declined 22% versus 15% for strength (Alcazar et al., 2023). PowerFrail converts chair-rise performance into watts/kg, with strong validation metrics (ICC 0.84–0.92).
Early pilot models suggest multi-metric screens outperform any single test, but large validation cohorts are still underway.
Clinical Implementation: Deploying the Biomarker Toolkit
Screening: Every adult ≥ 50 years should be screened with handgrip, 4-m gait, and 5-STS power tests (~2 minutes total).
Risk Stratification: Red flags include gait ≤ 0.8 m/s, grip below sex-specific cut-offs, or power < 1.5 W/kg.
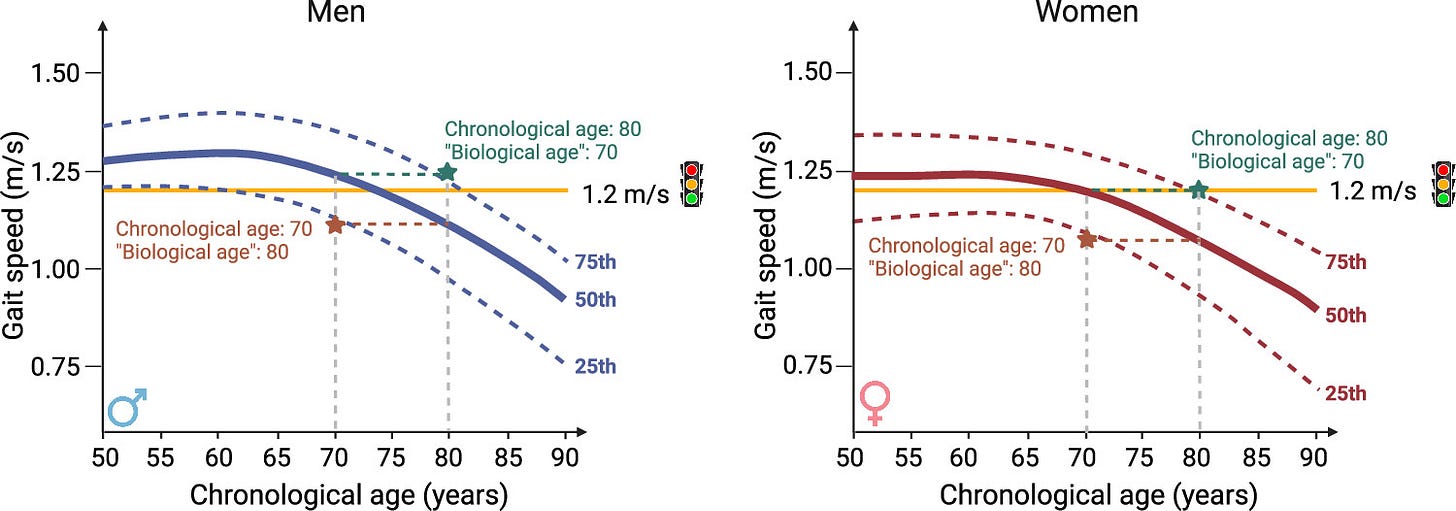
Intervention: Early interventions such as high-velocity resistance training, progressive walking programs, and protein optimization improve function and molecular aging markers. Exercise has been shown to shift epigenetic aging clocks (PhenoAge) by 1–3% toward a younger profile (Murach et al., 2022; Xu et al., 2023).
Monitoring: Functional scores improve faster than laboratory markers, providing timely feedback to patients and demonstrating return on investment to payers.
Next Steps in the Series
Future installments will explore molecular hallmarks of aging (telomeres, methylation clocks, SASP) and integrate functional and molecular data into a clinic-ready aging index.
Summary
This evidence-based approach advocates for a paradigm shift in primary and vascular care: replacing chronological age with rapid, objective functional biomarkers to better predict outcomes, personalize treatment, and optimize healthspan.
References
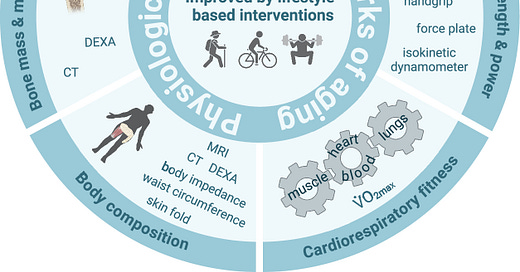
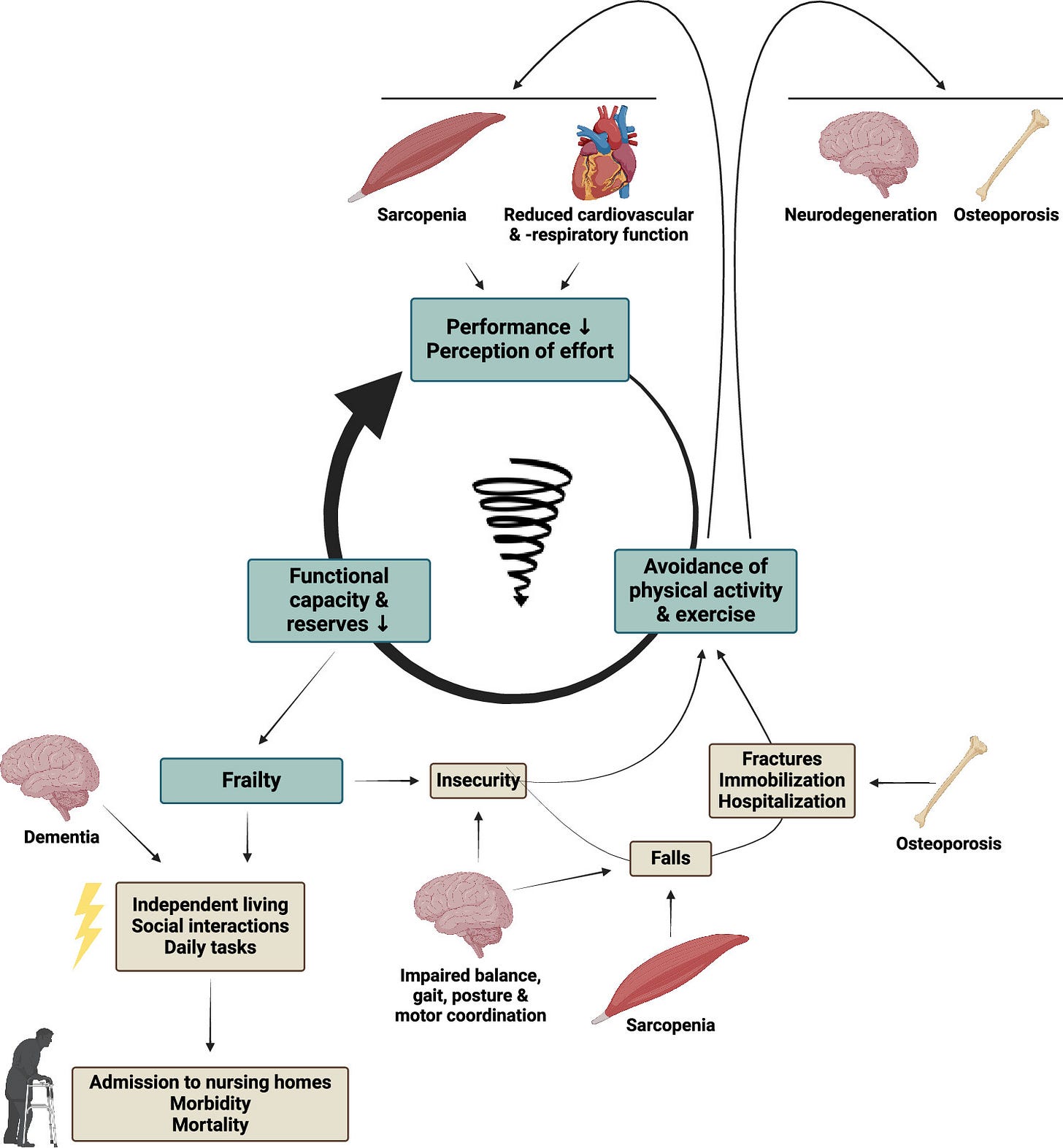
This post was inspired by “Biomarkers of aging: from molecules and surrogates to physiology and function.” All images come from that study.
Furrer R, Handschin C. Biomarkers of aging: from molecules and surrogates to physiology and function. Physiol Rev. 2025;105(3):1609-1694. doi:10.1152/physrev.00045.2024
Other References
Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50-58. doi:10.1001/jama.2010.1923
Yoshida D, Kaminaga K, Kimura M, et al. Preoperative handgrip strength predicts postoperative pulmonary complications in older surgical patients. Anesth Analg. 2020;131(3):838-846. doi:10.1213/ANE.0000000000004911
Kim DH, Kim CA, Placide S, et al. Prevalence of frailty and its association with healthcare resource use in older adults. J Am Med Dir Assoc. 2020;21(5):458-462.e2. doi:10.1016/j.jamda.2020.01.015
Kunadian V, Qiu W, Lagergren M, et al. Frailty and healthcare costs after invasive cardiac procedures. Eur Heart J Qual Care Clin Outcomes. 2019;5(3):161-168. doi:10.1093/ehjqcco/qcz023
Lee MR, Jung SM, Bang H, et al. Handgrip strength and cardiovascular mortality in half a million UK Biobank participants. BMJ. 2022;378:e070322. doi:10.1136/bmj-2022-070322
Alcazar J, Kamper RS, Aagaard P, Suetta C. Ten-year decline in lower-limb power outpaces strength loss and predicts disability and mortality in older adults. J Cachexia Sarcopenia Muscle. 2023;14(2):428-439. doi:10.1002/jcsm.13123
Muñoz-Arranz G, Alcazar J, Roldán-Gutiérrez A, et al. Smartphone-based five-repetition sit-to-stand power test detects sarcopenia in community-dwelling older adults. Exp Gerontol. 2023;173:112056. doi:10.1016/j.exger.2023.112056
Murach KA, Rogowski LA, Holmes SA, et al. Weighted-wheel running attenuates skeletal-muscle epigenetic aging. Aging Cell. 2022;21(7):e13657. doi:10.1111/acel.13657
Xu C, Perkins GA, Geoghegan F, et al. Aerobic training resets skeletal-muscle DNA-methylation landscape in cancer survivors. FASEB J. 2023;37(4):e23145. doi:10.1096/fj.202201220R
If you want, I can help you draft a professional Substack post or clinician resource based on this content. Would you like that?